
Failure to prepare for a pandemic alongside chronic underfunding was to blame for many avoidable deaths from COVID-19, the People’s Covid Inquiry heard last night.
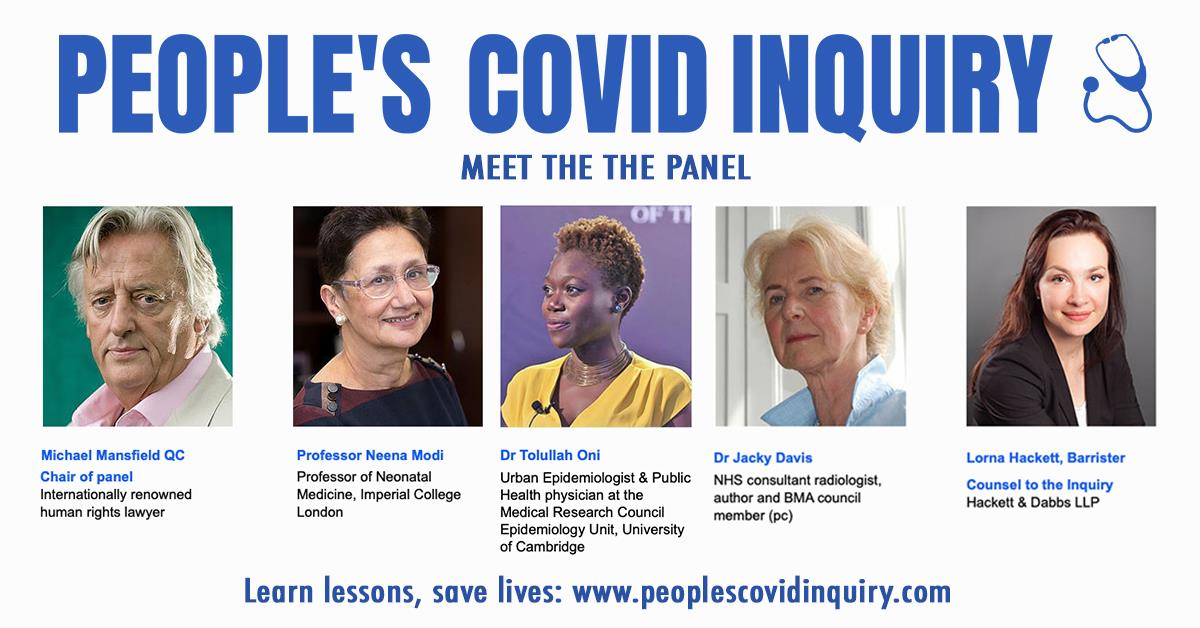
In the first of eight sessions, the People’s Covid Inquiry asked: how well-prepared was the NHS was to deal with a pandemic, in a discussion broadcast to an online audience. The impressive panel, led by Michael Mansfield QC and including our own Dr Jacky Davis, heard from expert and citizen witnesses about their experiences relating to the preparedness of the NHS last spring.
The Inquiry - so important with no sign of any official public inquiry - is the first people's inquiry of its kind to be held exclusively online, due to the constraints of the COVID-19 pandemic, and the first session is now available to view online on YouTube.
Inability to respond to COVID-19 impact
The first witness to speak was Jo Goodman, founder of the group Bereaved Families for Justice, whose father died after he contracted COVID-19, very likely at a crowded outpatient clinic where there was inadequate advice or protection from coronavirus.
She also told the panel of difficulties her member families had accessing hospital care: “Really early on, one of the clear patterns emerging was of people clearly needing hospital treatment but were told to stay at home by the 111 service.
“At the outset of the pandemic the 111-coronavirus service was outsourced to a number of companies and there was very, very limited training compared to the normal 111 service.”
She added: “I lost my dad. He was one of those that lost his life because the lockdown came too late and because vulnerable people weren’t effectively protected. My dad received his shielding letter 9 days after he passed away.”
Goodman explained how she set up the Bereaved Families for Justice Group as she believed her father’s death to have been preventable. The group now has 2,600 members, all with similar personal experiences.
The panel of experts included Professor Neena Modi, Dr Tolullah Oni, Dr Jacky Davis and featured counsel to the Inquiry barrister Lorna Hackett and chair Michael Mansfield QC.
Providing evidence of the experiences of NHS staff was Holly Turner RN, a children’s mental health nurse for CAMHS.
She told the panel: “Personally, I was not aware of any [discussions on preparedness for a pandemic] and building up to the start of this pandemic at the beginning of 2020 there weren't discussions.
“But I think all the services are so stretched, just getting your day-to-day work done there is too much-limited capacity to be thinking about anything else.”
She also pointed out the significance of the impact of the lack of preparedness on children and their families, even if they weren’t affected by COVID-19 directly.
“These children rely on routine and continuity, predictability, and that is all the things that support them in being emotionally stable, and everything was completely taken away from them: their school, respite, carers coming into help their families at home. They just went into complete crisis and we couldn’t go in to see them as the risk of covid was just too high.”
Turner pointed to the fact the vaccine roll-out has been a success as proof that the NHS is able to function well, and the committed staff able to deliver, when provisions are made saying: “The vaccine rollout is evidence that when the NHS has the resources, they can get the job done.”
A lost decade of cuts
The panel also questioned Professor Sir Michael Marmot, a health inequalities expert who published the Build Back Fairer: The COVID-19 Marmot Review at the end of last year. He argued that reduction in healthcare spending since 2010 had been behind the lack of preparedness.
“Government say they protected the NHS spending but it had gone up 3.8% annually and [then] went up 1%, that is equivalent to a cut,” he said, as prior to 2010 annual spending growth on the NHS had been around 7% which is necessary to keep up with demand.
Government policy reflected an attitude of “the greater the need, the greater the reduction in spending,” he added.
Expert witness Professor Gabriel Scally, President of Epidemiology and Public Health Section of the Royal Society of Medicine, and member of Independent SAGE, gave evidence that backed this up.
“All the [public health] contingency planning and contingency system was stripped out after 2010. The regional function disappeared. Local functions had a huge amount of resource stripped out from them.
“I think we would have coped much, much better absolutely [without contingency planning being stripped out],” he said.
The People’s Covid Inquiry panel will hear all eight sessions of the Inquiry, the next of which will ask: How did the Government respond?
Dr John Lister academic and campaigning journalist, editor of Health Campaigns Together ended the session with a body of evidence highlighting the damage to the NHS and social care of a decade of austerity and outsourcing.
All statements and supporting documentation will be on the Inquiry website very soon.
Find out more
You can find out more about the session and sign up on the People’s Covid Inquiry website.
The first session is available to view on YouTube and evidence presented to the Inquiry in the first session will be available on the People’s Covid Inquiry website shortly.






Leave a Reply