
It’s not even winter yet, but the NHS is already in a major beds crisis and bracing for the worst as Chancellor and new PM mull over the extent to more public spending cuts.
John Lister writes in this article from The Lowdown
Far from growing to meet demand, the most recent inflation forecasts show that England’s NHS budget in 2025 will be over £4 billion SMALLER in real terms than it was last year, and £12 billion smaller than promised by Rishi Sunak as Chancellor a year ago – and as The Lowdown has warned, local health services across England, now carved up into just 42 “Integrated Care Systems” have to generate unprecedented ‘savings’ (i.e. cuts) this year and next.
The result is a funding squeeze as bad as the Thatcher years in the 1980s. NHS England’s normally docile Chief executive Amanda Pritchard has gone on record to warn that before any further cuts “the money is a f**king nightmare.”
Ben Zaranko of the Institute for Fiscal Studies told the Health Service Journal the financial squeeze is the tightest-ever: “only seven times in the entire history of the NHS has real-terms budget growth dipped below zero, and not since the early 1950s has it done so in two consecutive years.”
NHS Providers interim chief executive Saffron Cordery says: “There is absolutely no financial wriggle room to stretch the budget even further without this having knock-on effects for health and care.”
It’s so bad even the NHS Confederation is warning that any further erosion of an already inadequate NHS budget will endanger patients:
“Exceptional inflationary pressures in recent months and other unexpected cost pressures have already left the NHS facing a £7bn gap in the budget next year compared to that set out in the 2021 spending review. This funding gap will already have to be made up by some key areas of planned expenditure being delayed.
“With 132,000 staff vacancies, a waiting list of over 7 million and other areas of care under huge pressure, … the NHS will be plunged into an unsustainable crisis if local services are asked to go any further in finding efficiency savings.”
The Confed’s CEO Matthew Taylor added:
“There is now a real and present danger to the NHS. Anyone who thinks that further public sector funding cuts won’t have a direct impact on patient care and safety is living in fantasy land.”
So desperate are the times that the editor of the Health Service Journal, Alastair McLellan, issued an unprecedented call for local NHS trust chief executives and Integrated Health Board chairs to lobby local Tory MPs in advance of the expected Halloween budget statement.
But even the HSJ call to action falls short of what’s needed to defend the NHS. The situation is so bad that just stopping any further funding cuts is nowhere near enough: front line capacity is already inadequate, with services under massive strain on all fronts.
The latest annual report from the Care Quality Commission sums up the state of “gridlock” created by over a decade of austerity and real terms cuts in NHS funding:
“Our health and care system is in gridlock.
“People in need of urgent care are at increased risk of harm due to long delays in ambulance response times, waiting in ambulances outside hospitals and long waiting times for triage in emergency departments.
… “People’s inability to access primary care services is exacerbating the high pressure on urgent and emergency care services.
… “Public satisfaction with NHS health care and with social care has plummeted in 2021/22.”
With over 9,000 acute beds (almost one bed in ten) occupied by Covid patients on October 26, NHS England has warned that up to half of all hospitals beds in England could be occupied by patients with respiratory infections, including Covid and flu. 12,000 more beds each day on average are filled with patients who cannot be discharged for lack of social care – putting one in five front-line beds out of use for emergencies or elective care.
NHS England, who appear to have given up on pressing for funding to match demand, and saying nothing about grossly inadequate numbers of beds and staff, have announced they will be setting up regional “war rooms” to keep track on the hospitals under most pressure. They hope to divert some patients away from the hottest spots – but at risk of leaving patients stranded many miles from their homes, with much more complex problems discharging them later.
Heart specialists are warning that response times have been increased and services for heart attack victims are a shambles because of bed shortages, ambulance delays and logjams in A&E departments.
Frustrated ambulance chiefs warn that in September alone 38,000 people may have been harmed by long delays in handing patients over to A&E staff, and 4,100 potentially suffering “severe harm”.
Reports from Cornwall, Salisbury and Portsmouth in the south to Hereford in the midlands, Greater Manchester in the north west, Hull in Yorkshire and Blyth in the north east tell the same story of overwhelmed hospitals and swamped emergency departments, with management increasingly expressing their fears for the consequences to patients.
In Aintree Hospital in Liverpool the hospital’s main corridor has been converted into a makeshift ward, after the corridors of its emergency department had already been filled with patients waiting to be admitted to a ward.
Meanwhile hospital bosses in Worcester say that despite previous criticism of delivering care in corridors they again feel forced to choose between treating patients in corridors or in the back of ambulances. The Trust says it is short of 45 beds, leaving 20 people a night waiting in A&E.
In a meagre response to the unprecedented crisis Rishi Sunak toured Croydon hospital wards, only to be chastised by one female patient for not doing more on NHS staff pay. He was also forced to abandon his ‘big idea’ – to fine patients £10 for missing doctors appointments, which the BMA condemned as unworkable and counter-productive.
Sunak’s spring budget only a few months ago effectively doubled NHS efficiency targets from 1.1% to 2.2% a year, without any regard for how achievable this might be. And it’s now clear that far from freeing up any extra resources to fund priority areas of the health service, any savings will be swallowed up at once by inflation as NHS chiefs debate which services to cut back.
In January the SOSNHS campaign, linking health campaigners with trade unions and political organisations committed to defend the NHS, took up the call for an emergency cash injection of £20bn to help put England’s crisis-ridden NHS back on its feet. It was seen as a down payment, beginning the process of unrolling a decade of austerity and returning to the performance levels of 2010, when David Cameron’s coalition government first slammed the brakes on spending and began the long painful decline.
£20bn now seems an even more modest amount – barely enough to compensate for inflation and the real terms cutbacks already under way: but it’s vital that campaigners start to bang the drum loudly for a big, immediate increase in NHS funding as Jeremy Hunt prepares his autumn budget.
John Lister is co-editor of The Lowdown and Health Campaigns Together Committee/KONP member
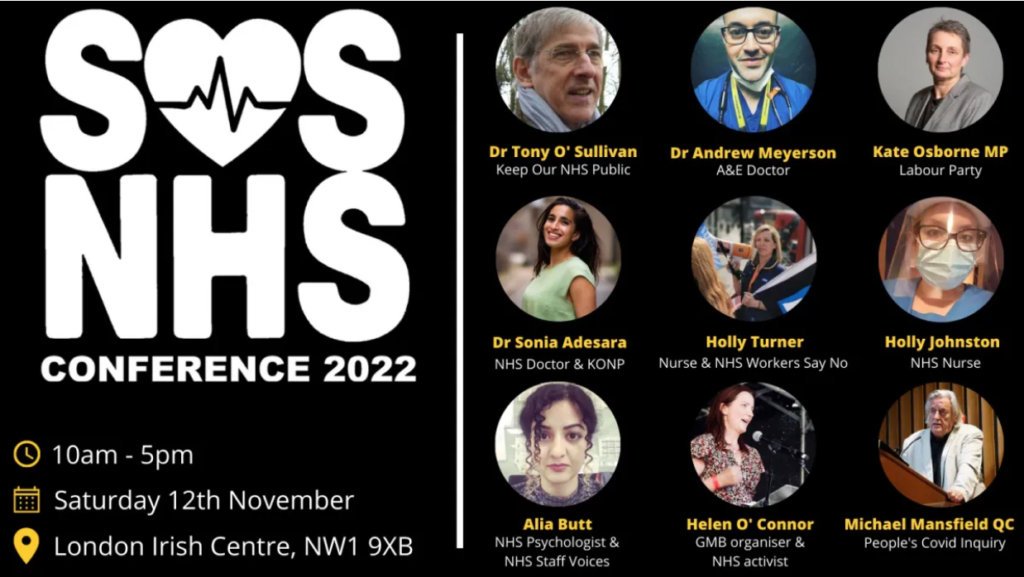
SOSNHS is holding an important conference in person and online on November 12
Information HERE.

Leave a Reply