
Liverpool Hospital has been at the heart of the second COVID wave as infection rates have been soaring at alarming rates since the start of September reports frontline medic, Dr Rory Hicks
At the Royal Liverpool University Trust the hospital is already at full capacity with multiple COVID wards being full meaning sick patients are waiting for a bed in A/E. In addition, with winter fast approaching there is going to be a huge demand for medical beds and need to isolate and care for seasonal flu patients. Liverpool and many other northern city hospitals have been left to fend for themselves and abandoned by the government until far too late leading to the COVID pandemic spiraling out of control once again.
Currently, Liverpool has a brand-new hospital that has been in the building process for several years and as a result of the collapse of the building firm Carillion and the refusal of the Conservatives to fund its completion it still lies empty.
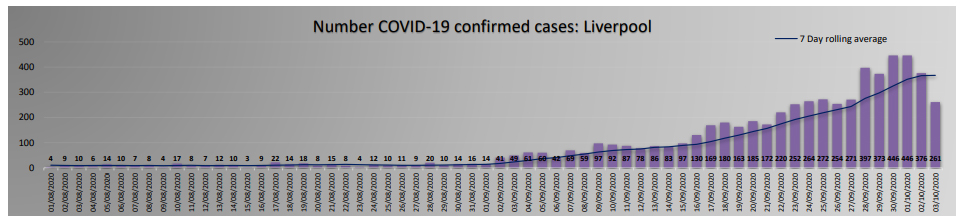
Since the 1st of September, there has been a rapid and worrying increase in the number of COVID 19 cases in Liverpool. Numbers climbed from 94 cases per week to the current level of 2570 cases per week. Local data covering testing up to the 16th October 2020 show that the total number of confirmed cases for the last 7 days is 2825. This gave a weekly rate of COVID-19 in Liverpool of 567.2 per 100,000 population and a positivity testing rate of 19.4%. This rate has continued to dramatically increase and on Wednesday 13th October the new “tier 3” measures were enforced in Liverpool by the government.
The second wave of COVID 19 was unfortunately very predictable and something many medical professionals knew was going to occur. Students have returned to schools and universities, pubs, restaurants, hairdressers have reopened, and people have been encouraged to return to work, often without sufficient measures being taken to protect staff e.g. no personal protective equipment being provided.
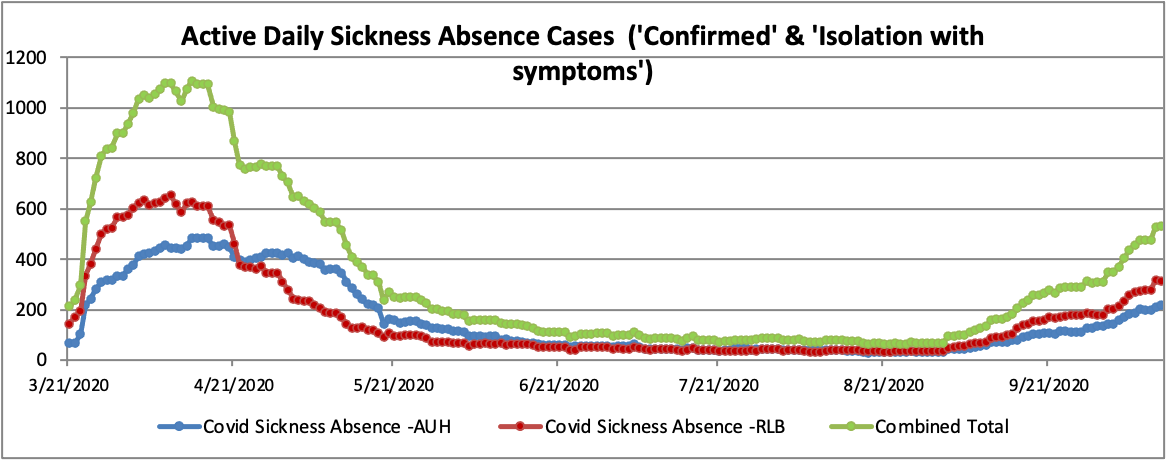
During the first wave of COVID 19 numbers increased dramatically in Liverpool from early March, peaking in April. The epidemic put extreme pressures on the hospital stretching it to its capacity. Guidance was given to hospitals from Public Health England to take dramatic actions to try and prepare the hospital for the surge in hospital admissions.
- All surgery apart from emergencies and outpatient clinic appointments were cancelled.
- Staff were reallocated to provide support where needed.
- Surgeons and radiographers were responsible for medical wards caring for COVID patients.
- Dentists and secretaries were trained to ensure appropriate PPE was being worn by staff and used on all wards.
- Academics and retired physicians were asked return to work in hospitals to provide care for COVID patients.
Hospital beds were mainly occupied by COVID positive patients however, overall we saw a decrease in hospital bed occupancy with many common medical conditions such as heart attacks or strokes not present in the numbers that are usually seen.
Comparing this to the now established second wave there are some very worrying differences that will stretch our hospitals even further and I wonder if they will be able cope.
- The NHS/ local trusts are desperately trying to catch up on the back log of missed outpatient appointments and elective surgeries. As a result they have not been keen to announce further measures to restrict or reduce this until absolutely necessary.
- Despite local numbers rising since September, little has changed within the hospital. Only this week certain elective operations have been cancelled and outpatient clinic numbers reduced.
- The number of staff on sickness-leave or self-isolating is dramatically increasing meaning there is less people available to care for an ever-increasing number of patients.
- This time round there will be no redeployment of other specialties (surgeons, dentists, academics, retired physicians) to assist in the increased need for medical beds. This has already led to medical physicians being over stretched in managing the care of multiple medical wards.
- Worryingly, hospital beds are already fully occupied with general medical conditions that we did not have to manage during the first wave. Subsequently, we do not have sufficient bed space or staff to care for the ever-increasing number of COVID patients.
Something we saw during the first wave is already occurring; medical staff across the board are “burnt out” and fatigued. Most have not been able to take annual leave and fully recover from the emotional stress inflicted from seeing so many patients suffer with this illness. Rotas have been put in place to try and cope with the huge surge in demand for medical care. As a result, staff are being asked to work extra shifts to desperately try to cover the numerous gaps.
The most worrying aspect and difference of this second wave of COVID-19 is unfortunately the timing. Every winter the NHS is put under severe pressure with an increase in hospital admissions demanding more medical beds. With flu season rapidly approaching there will be an increased need for testing from laboratory services and we will have to isolate more sick patients with medical conditions other than COVID-19. This second wave will stretch hospitals further than ever before, leading to an overwhelmed health service, exhausted staff and sadly may result in patients receiving worse medical care.
Chancellor of the Exchequer Rishi Sunak stated that there would be a ‘blank cheque for whatever it takes for the NHS’ and yet staff on the front line have not seen any of this. Nightingale hospitals have been created to increase the number of beds but there are not enough staff to care for the unwell patients in the hospitals we already have. We need to stop the “smash and grab” privatisation of NHS services to private (often shell) companies, many of which have won contracts with no competitive tenders.
We must demand urgent investment in our massively underfunded NHS, more staff to be trained and for nurses and other allied health care professionals to have a fair wage and not be crippled in debt from their university fees.
Dr Rory Hicks locum infectious disease registrar






I am so proud of all staff in our NHS like this Dr, who keep on working despite the lies the government and the pathetic opposition keep spewing out. What is wrong with US why are we just taking this? We are being told by staff on the front line that they do not have the equipment they need, the staff they need, we are being treated like absolute fools by those in power. We are the donkeys and I don’t want to be an ass any longer I want to fight for Rory