
National KONP and NHS News
Keep Our NHS Public says no to NHS England’s Long Term Plan
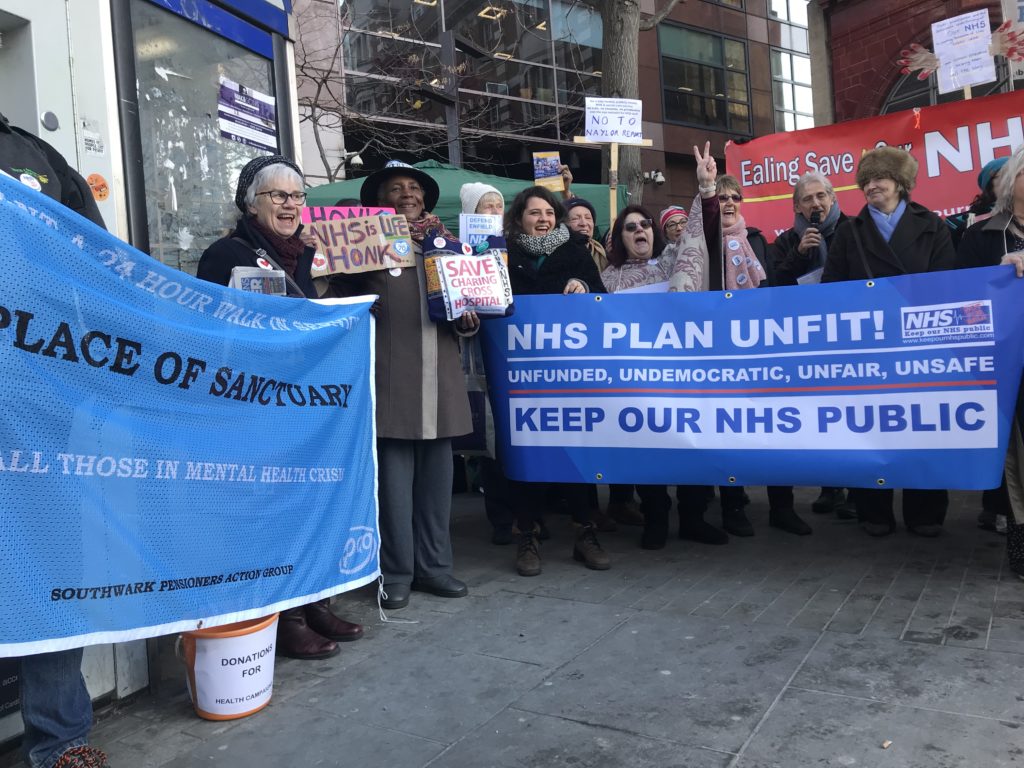
On the chilly morning of Thursday 31st January, KONP held a rally to demonstrate against the government’s and NHS England’s NHS Long Term Plan which has uncosted and therefore grandiose plans, without a realistic plan to staff them. The plan threatens an imposed top-down reorganisation with risks of future large-scale privatisation, further cuts to our health service and a damaging sell-off of NHS land. The rally was held in front of Skipton House (next to Elephant and Castle tube station) while, inside the building, an NHS England board meeting was taking place to discuss the Long Term Plan.
Tony O’Sullivan, Co-Chair of KONP led the rally with an informative flow of speeches explaining the facts, figures and shenanigans of successive governments’ attempts to destroy our health service as a public body. This took place against a back-drop of banners and a marquee, set up by Tom Griffiths (Campaigns Officer, KONP). There was a good response from the public as they took leaflets on their way to work. Passing traffic including buses added their honks, and some drivers even took leaflets supporting the campaign. There were many very good speeches from from amongst Lambeth, Lewisham, Ealing, Hammersmith & Charing Cross, Enfield, Southwark and Greenwich campaigners, with their banners and hand-made placards.
The Long Term Plan is grossly unfair and unsafe. The main substance of the plan of what has been published or leaked are simply a re-run of previous plans:
- The Conservative government and NHS England claim the plan, which includes 60 totally uncosted proposals, will improve long term care.
- With sweeping and undemocratic mergers and enabling new legal changes, local communities are at risk of losing both local access to care and their rights to hold their local NHS to account.
- Patient access to a doctor is being drastically reduced as GP practices are being cut from 7500 to just 1500 so-called ‘super practices’.
- NHS bodies in each of 44 areas must create an Integrated Care System (ICS) by 2020, and legal changes will be made to enable private tenders for ICS contracts.
- All local clinical commissioning groups (CCGs) in each ICS area are being told to merge – greatly restricting the public’s right to be consulted and to challenge individual CCGs. Local authority Scrutiny Panels will struggle to scrutinise, as is their right.
- Each ICS will form a new Integrated Care Provider (ICP) organisation, and any wholly NHS alliance will most likely to be competing for the contract with private companies or joint public (NHS)/private partnership.
- Under current law, the performance of providers in these contracts is not accountable to public scrutiny, and many private healthcare companies already specialise in limiting eligibility to healthcare.
- If large commercial companies are awarded long term £multi-billion contracts, our NHS will become fully ‘financialised’ – run by and for commercial interests – and restrictions to healthcare and rationing will be speeded up.
The consequences of this unfunded Long Term Plan is a 10-year plan to maximise private revenue and reduce public costs to healthcare, and will result in cutting access to a wide range of health treatments in drastically fewer settings. Migrants and other people judged to be ineligible for free NHS treatment will be charged. NHS trusts will be told to increase income through private health and insurance. We must unite against the government’s plan, commercial contracts have no place in a health service for the people; we don’t want Integrated Care Providers, we want a publicly funded, publicly provided and publicly accountable National Health Service. We want the end of privatisation of the NHS.
Report from Ellen Graubert of Hackney KONP.
For more information on the Long Term Plan see our report below.
________________________________________________________
NHS Long Term Plan – unfunded, undemocratic, unfair, unsafe
It’s tempting to dismiss the NHS Long Term Plan, published on January 7 by NHS England, as an unrealistic wish list of developments completely divorced from the real constraints on resources. But it demands close analysis. There may be some messages that cannot be dismissed but they distract from the meat of the Plan. What is shocking is the virtual absence of discussion and proposals to address the severe problems facing the NHS. The major restructuring of the NHS goes forward at pace.
NHS England’s proposals will request that the government rescind regulations enforcing contracting requirements of the 2012 Health and Social Care Act that make CCGs parcel up services and put them out to competitive tender. This is a way of reducing the current market chaos 1000s of contracts in health care bring. But it does not by any stretch mean the exclusion of private profit – bigger centralised budgets may be up for grabs.
It is impossible to discuss the Plan’s content without also addressing the vital issues that are omitted from it and the diversionary list of service improvements that it freely promises.
Some positive concessions and considerable window dressing
There are a few positive concessions to the pressure of campaigners and the needs of patients:
- new waiting time targets are to be introduced for adult and child mental health, and funding is to be preferentially allocated to mental health – although with insufficient funding in total this implies cutbacks elsewhere;
- action to address unexplained mortality for people with learning disability and autism and the long waits they experience;
- Unlike many previous plans there is no explicit call to close acute hospital beds even if alternative services reduce demand for them – in order to scale down bed occupancy and stress on front line staff;
- There is even discussion of health inequalities;
- The idea is floated that the NHS take back responsibility for some public health.
And there is promise after promise of prompt response services, proactive care, flexible teams, neighbourhood teams, primary and community care teams, community multidisciplinary teams and upgraded support – all in happy-clappy, completely abstract terms.
Missing from the Long term Plan

The number of major issues that are either ignored completely or blithely brushed aside in the 136-page Plan is certainly enormous: they include the declining actual performance of trusts; the inexorable rise in emergency caseload; the insufficient capacity in acute and mental health services and bed shortages; the disastrous financial plight of most acute trusts; the workforce crisis compounded by the Brexodus of EU-trained staff; the £8 billion and rising bill for backlog maintenance; the damaging cuts previously inflicted in mental health and those ongoing in community services; the cuts in public health budgets; the widening gap in society between rich and poor and the resultant inequalities in health – exacerbated by unchanged austerity and reactionary government policies on housing, welfare, education, and local government: and of course the gathering crisis of a dysfunctional social care system.
The Plan, and its preceding Operational Planning and Contractingdocument, published on December 21, concede that they are incomplete: no workforce plan has yet been published, and there is no evidence to suggest that work on this has advanced at all; the “framework for implementation” is promised for “spring” – presumably spring 2019.
Moreover while we know from every informed observer that the famous £20.5 billion “extra” funding over five years announced three times last year is not enough to do much more than stabilise the NHS and keep the lights on, the amount of capital available to fund any substantial new projects will not be known until the Autumn Spending Review.
Nonetheless the December document outlined a break-neck pace for a clearly impossibly ambitious timetable for changes: the first deadline (14 January) for major decisions has already passed – just a week after publication of the Long Term Plan and 13 working days after the December document appeared. Managers are already running just to catch up.
With wholly inadequate funds, over 100,000 staff vacancies and no serious implementation plan, the Long Term Plan has to say something, and so it rattles out upwards of 60 uncosted commitments to improve, expand or establish new services, most of which if taken at face value would be most welcome – but which taken together in this context are completely unaffordable, unrealistic and incapable of implementation.
John Lister, co-chair KONP and Editor of Health Campaigns Together
________________________________________________________
We’re Hiring: National Administrator at Keep Our NHS Public

We are currently looking to recruit a London-based, friendly, committed and enthusiastic administrator in our national office. This key role is all about ensuring that KONP’s campaigning can have the biggest effect possible by providing us with essential administrative support. The role involves being the first point of contact for people who engage with our campaign, offering assistance to community and national campaigners and the KONP team. Other roles include managing the KONP online shop, managing our group and membership subscriptions, managing alongside the campaigns officer and others and assisting in organising events to build the campaign. You can find out more here.
We’re a small organisation with a big agenda and need a national administrator who is, friendly, positive and calm in dealing with urgent matters, prioritises tasks well and enjoys problem solving. If you’re interested or know anyone who is, please forward them this link and ask them to apply by emailing, [email protected]
Application deadline: Friday 22 February (end of day)
________________________________________________________
Challenging and Supporting Local Councils (Briefing No.2)
- Some Councils refused to sign off the STP.
- One Labour Council Health portfolio holder didn’t understand his brief: once we had enlightened him, he put forward much better proposals.
- One Conservative Council Scrutiny Committee, under pressure from their Electorate and KONP campaigners vigorously challenged the STP Footprint’s Health Managers again
We’d be interested in your experiences.
‘We were right’ say Junior Doctors as unsafe contract laid bare.
Two years after the first all out doctors’ strike in British history the effects of this government-imposed contract have been published. The first figures since then, revealed by the Health Service Journal earlier this week, show the results of this unpopular and unsafe contract upon the NHS workforce. Striking Junior Doctors who opposed it say, ‘we were right’.
Data shows that around 36,000 junior doctors in England have worked beyond their contracted hours more than 63,000 times since 2015. Approximately the same number of doctors have also filed exception reports to draw attention to unsafe staffing. The ability to complete and file these reports is a power clinicians were afforded after the dispute, presumably in order to try and mitigate the fallout.
 Why did doctors walk out?
Why did doctors walk out?
In September 2016 junior doctors stood up to say no to a contract that demanded they stretch a 5-day service into 7 with no extra capacity. The strikes, (part of a contract dispute which began in 2013), were a watershed moment. The strikes highlighted the distinction between the government’s attitude towards the NHS and the reality for those on the front line, (both staff and patients alike).
Over 20,000 doctors on almost 150 picket lines across the country participated in industrial action to warn against the imposition of increasingly unsafe working practices. Sadly, their pleas and efforts to ensure patient safety fell on deaf ears and after a valiant collective effort the contract was nevertheless imposed.
Junior Doctor Aislinn Macklin-Doherty, also Secretary of Health Campaigns Together, told Keep Our NHS Public,
I was a junior doctor when Jeremy Hunt imposed this contract on us in 2016 and I am still a junior doctor now. I fought against it. I stood outside my hospital in the cold and rain to fight for high quality care for my patients. And I am now seeing the disastrous effects of this imposition 2 years on. We said there weren’t enough doctors to look after patients for longer hours. We were right. We said trying to make us do even more with even less of us would be dangerous. We were right. We said that it would lead to patients lives being put at risk. We were right.
The treatment we doctors and also my nursing and other NHS colleagues have received at the hands of this government is unforgivable. But most of all it is unforgivable how patients have been treated. This Govt have made political choices that have costs lives.
Unsafe staffing
The resulting process of the ability to submit exception reports is at least a way to highlight potentially dangerous working conditions. Worryingly though, some senior members of staff discourage submitting them as it can make the department appear inefficient. There are significant and concerning consequences of an underfunded and understaffed system (100,000 NHS vacancies including 11,000 doctors), and simply fining hospital trusts for the effect of a lack of staff is tantamount to shifting the deckchairs about on the Titanic. Circumstances will not improve unless there is a mass successful implementation of staffing across the board.
Trusts are supposed to offer time off in lieu or additional financial incentives for extra hours worked and ultimately to address the issues leading to repetitive overtime. Since 2016 there is now a specific position assigned to deal with this problem, (which in itself is a clear sign of the times). A ‘Guardian of Safe Working’ at each trust decides if trainees are working unreasonably long hours.

Scapegoats for government mismanagement
There is of course greater potential for error in a system with no slack; in a service that is chronically understaffed and underfunded, where rota gaps are the norm and ‘corridor nurses’ are an established position. Successive governments have, by running the NHS into the ground, also created a culture of fear amongst clinicians.
They are contractually obliged to keep quiet. This ever-present fear should in no way be viewed as an accidental by-product, but as a deliberate method of control. Whistle-blowers like Dr Chris Day are treated appallingly and are shown up as an example of what will happen should workers dare to publicly express an opinion.
Not only are those who highlight legitimate safety concerns treated unfavourably, they are attacked. NHS England recently spent £700,000 of taxpayer’s money on trying to silence Dr Chris Day when he took them to court over inadequate staffing at his hospital that was creating an unsafe working environment. This government body therefore was actively working against improving patient and staff safety. There are serious and sinister undertones here that should not be disregarded.
Junior doctor, Sonia Adesara told us:
Everyone is working with rota gaps so therefore doctors have to works longer hours to ensure patient safety is maintained. Doctors are doing this on a regular basis. Management have already tried to make ‘Exception Reporting’ difficult to do as they say our consultant has to sign it off, this makes it very difficult for trainees to do. If there wasn’t so much fear I think the numbers would be even higher than this in my opinion.
Samantha Wathen,
Press Officer
Keep Our NHS Public
Local Group News
Theresa May’s launch of the NHS Long Term Plan should fool no-one in Liverpool or anywhere else.

Theresa May was welcomed to Liverpool by Merseyside KONP, Save Liverpool Women’s Hospital campaign and a hundred protestors who gave her a very clear message on her plan.
Despite the mild weather, the Royal Liverpool has been on ‘Red Alert’ at least 25 times since 1 December. Bed occupancy is 92.3%, against a safe level of 85%. In December, 495 ambulances waited over 30 minutes to discharge their patients, and 135 of these waited over 60 minutes. Last week, some patients waited over 3 hours to be seen in A&E, and some in A&E waited 24 hours for a hospital bed.
Why? The half-built Carillion PFI hospital was designed with fewer beds and capacity at the Royal was cut to match the plans. The Trust justified the cuts, claiming that Care in the Community would reduce demand.
May’s plan, written by NHS England Chief Exec Simon Stevens, will replicate this all over England, shifting resources out of hospital, promoting digital technology and telling patients to look after themselves.
 Rationing
Rationing
Last winter, former Health Secretary Jeremy Hunt suddenly postponed all elective (planned) operations to ease the pressure on hospitals. Now, an NHS England document Preparing for 2019/20 Operational Planning and Contracting intends to ensure that ‘as much of [sic] inpatient elective activity occurs in the first half of the year, before winter’.
The document also includes a rationing plan for 17 NHS treatments no longer to be commissioned by CCGs. Trusts are also urged to ‘grow their external (non-NHS) income’ and ‘work towards securing the benchmarked potential for commercial income growth’. They must set up systems to raise money by charging patients for treatment (‘overseas visitor cost recovery’) – a policy recently denounced by several medical Royal Colleges because of its impact on individual and public health.
Long term agenda
The 44 discredited Sustainability and Transformation Plans, re-branded as Integrated Care Systems, will hold the regional budgets to control NHS Trusts. ‘Planning assumptions’ in each STP area are to be agreed by 14 January. Neither the STPs, nor the ICSs, nor the Long Term Plan has been mandated by an Act of Parliament, let alone by patients or healthworkers.
The private sector could gain control of individual ICSs through long term contracts to manage the entire health system within one region.
Real integration of health and social care can only take place when the profit motive is taken out, with care fully-staffed and resourced, publicly accountable, funded through general taxation, and provided free at the point of need.
John Lister, editor of Health Campaigns Together said:
All of the main lines of what has been published or leaked about the Plan are a depressing re-run of previous plans and gimmicks: the only novel proposals are for more central control and less accountability, for trusts to run more like and with private businesses seeking profits, and to raise money by undermining the principles and values of the NHS through charging overseas visitors – a government policy widely condemned by NHS professional staff and campaigners as discriminatory and a step backwards from prevention and public health.
There is no reason to believe this plan, with even less local accountability and no serious plans for public consultation, will prove any more acceptable to the public or successful in implementation than the secretive STPs in 2016 or other previous failed efforts.
Campaigners have yet to see anything to recommend the new plans, or any indication NHS England is willing to come to grips with the crisis fuelled by chronic austerity limits on funding – or demand an end to chaos and fragmentation of the Health & Social Care Act.”
 Dr Tony O’Sullivan, KONP co-chair and retired consultant paediatrician, said:
Dr Tony O’Sullivan, KONP co-chair and retired consultant paediatrician, said:
The government has cut £7bn to social care and has underfunded the NHS by £20bn in annual funding over the last 9 years. There is no plan to repair the damage done. Platitudes about prevention and better health are exposed by the £1bn cuts to the public health budget responsible for prevention.
After 9 years undermining mental health, the ‘extra’ now committed is not new money but comes from elsewhere within NHS funding. Theresa May’s assertion that the NHS has never received higher funding is simply not true in relation to NHS funding required to meet need.
Over 210,000 vacancies in NHS and social care and unacceptable stress carried by staff, dangerous waits for A&E, cancer care and surgery, all tell the true story. And the fact that private health providers get 50% of their funds from treating patients diverted from an NHS deprived of the resources to treat them itself exposes the policy direction of government. We cannot accept this situation.’
We will be analysing the NHS Long Term Plan and sharing our more detailed views.
Dr Tony O’Sullivan
Upcoming Events
We’re very excited to announce the first meeting of a brand new Keep Our NHS Public Group in Southwark South London.
All those living, working or studying in Southwark are welcome
Date: Wednesday 27th February – 7pm-9pm Venue: 67 Balfour Street SE17 1PL
Please come to the founding meeting of Keep Our NHS Public for Southwark Speaker: Dr Tony O’Sullivan, National Co-Chair of KONP
________________________________________________________
Yorkshire Health Campaigns Together’s March for the NHS.
For more information contact Leeds Keep Our NHS Public
Saturday, 30th March – 11:30am
Leeds Art Gallery
The Headrow
Leeds
LS1 3AA
___________________________________________
Join KONP
Keep Our NHS Public is the longest running national and local membership campaign fighting to save our NHS. You can find out more about us here. By joining us you’ll become part of a community of health campaigners with unparalleled experience and passion, will belong to a nationwide network of activists and have the support of a core team of experienced organisers at a national level. It’s easy and doesn’t cost the earth. Join today.


Leave a Reply